Post-pandemic life: our digital habits, health care
In part three of a three-part series, Carolina experts discuss some lasting effects of the pandemic on digital technologies and health care.
Carolina’s Pandemic Year: This week last March, the University shifted to remote instruction. The Well is marking the occasion with a week of special stories, including ways the University has addressed the crisis, reflections from Chancellor Guskiewicz and, below, predictions from Carolina’s faculty on lasting changes to post-pandemic life.
Less travel, more virtual meetings. More protection of patient privacy to improve drug discoveries and medical care. New versions of home health care and psychiatric care provided to every North Carolina community.
These are some of the ways the pandemic has changed how we use digital technology and how we receive health care.
In the wake of this past year’s devastation, death and adaptation, The Well asked experts in various fields about how daily life may look different after the crisis lifts.
Virtual reality, data and diagnoses
Junier Oliva, assistant professor in the College of Arts & Sciences’ computer science department, is an expert on machine learning and artificial intelligence. He sees broad changes in the digital world stemming from the pandemic, starting with more demand for virtual meetings using the latest technologies.
“We are seeing that since there is little travel, one upside is that it’s much easier to invite folks to give a talk, meet with a class, do a seminar or a group or a happy hour. It’s a lot easier to do this virtually,” he said.

Junier Oliva
“I think generally people are connecting more virtually across the U.S. and beyond because there isn’t that expectation that you would bring someone in-person with all the associated overhead. That is something that may stick,” Oliva said.
Oliva said that computer scientists and industry leaders such as Xerox have been thinking about virtual meetings and collaborations for more than 50 years.
“It isn’t something that came out of the blue for computer scientists. As far as the latest and greatest innovations, I would imagine that things like virtual reality and augmented reality, virtual meetings and being able to collaborate remotely will be in demand,” Oliva said.
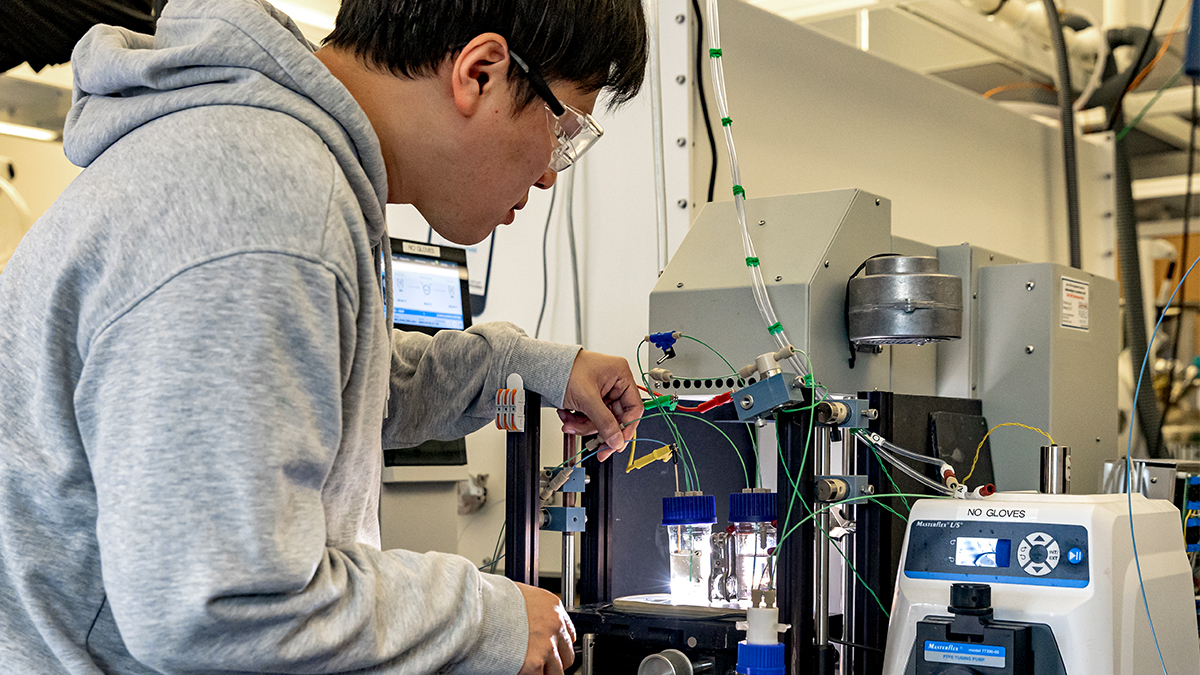
Another area that the pandemic accelerated is problem-solving with digital tools. Oliva is working on ways to take in sensitive medical data, then protect patient privacy by generating fake synthetic data that is useful for researchers without leaking private information.
“Once the pandemic hit, computer scientists were keen on solving some of the issues related to COVID-19. For example, I’ve been collaborating with folks trying to develop algorithms that can take in sensitive data related to health care, things that would be of interest to downstream researchers trying to make drug discoveries or trying to better diagnose patients. But, we can’t just release these data sets because they contain sensitive patient information.”
Even when no name is associated with a raw data record, a lot of information such as a person’s height or weight might allow for identification. “We’re looking for ways to perturb these values that would make it hard to track back features to one particular person and preserve their privacy,” Oliva said, referring to methods of replacing or distorting data so that unauthorized users cannot access it.
“For predicting if someone has COVID or trying to predict what drugs are going to be useful for a particular patient, it’s important to keep patterns intact as a whole in the data while perturbing and destroying any factorization that could be tracked back to an individual.”
Oliva said that computer scientists are also exploring digital means for less invasive medical procedures, more efficient COVID-19 testing and a machine-learning algorithm that can hear someone cough and predict whether the person has a certain illness.
New models of patient care
Dr. Ian B. Buchanan, president of ambulatory and post-acute care for UNC Health, is responsible for coordination of outpatient and continuing care in over 600 physician practices and at 12 hospitals.
Buchanan said that health care, normally a conservative, relatively slow to change industry, has experienced more flexibility and change in the past year.

Dr. Ian Buchanan
“Some changes have been really positive advancements, and some have simply been a response to the greatest public health crisis in 100 years,” he said. “We’ve had to adapt and do things and flex in ways that we never would have been willing to under other circumstances.
“The biggest sea change in terms of direct patient care that absolutely is going to stick is a recognition and a growing expectation by our patients that we care for them where they are. The pandemic is the first time in modern memory that people have felt really scared to go into health care settings. Our typical patient a year ago viewed our clinics and hospitals as safe places to be. Now, they’re concerned. ‘Gosh, who’s the person sitting next to me in the waiting room, and who is the person being wheeled past me in the hallway?’”
The confluence of patients’ expectations and maturing technologies brought an explosion in the amount of care that “we can provide and our patients would like us to provide when they’re not physically sitting in one of our clinics,” Buchanan said. And increased familiarity with using digital services for tasks such as ordering groceries makes people more comfortable interacting with health care providers via telemedicine.
Health care providers are engaging underserved populations in new ways. The pandemic has “laid bare existing inequities in health care delivery to minority, rural and underserved communities across the state and the nation,” Buchanan said. “That’s been a major focus for us throughout the pandemic.”
Increased telemedicine has created positive changes in psychiatric care that will benefit North Carolina, especially in communities without psychiatrists. “It’s no longer just folks who are able or willing to drive to Chapel Hill to see a psychiatrist,” Buchanan said. “We can provide psychiatry services across the state.”
Buchanan credits Dr. Samantha Meltzer-Brody, the UNC School of Medicine’s psychiatry department chair, with tailoring virtual care that has succeeded for physicians and their patients.
“Out of all the specialties in the state, we have per capita fewer psychiatrists than just about anything else. Even in a lot of medium-size communities, never mind small communities or rural areas, there are few or no psychiatric resources available,” Buchanan said.
UNC Health has enhanced home health care, building off a traditional model in which nurses evaluate and care for patients in homes. Buchanan said that new technology allows nurses to see and talk with patients, monitor their condition and also have immediate access to a physician.
That model enables patients to return home more quickly after hospitalization. It has also decreased emergency room visits because in situations that exceed a nurse’s licensure and normally require an ER visit, the nurse can contact a physician.
“We’re pushing the boundaries of our continuum of care at home,” Buchanan said.
This summer, UNC Health will begin admitting patients needing lower-acuity care into an at-home program. “It’s essentially a hospital admission, but in the patient’s home,” Buchanan said. “Nurses and physicians at a command center will monitor patients at all times. Patients will have all the resources available in their home for their nursing care, respiratory care and pharmacy needs.
“Patients who are relatively lower acuity move to the comfort and safety of their home while freeing up hospital beds,” Buchanan said. “It’s a much less expensive care model, which is good for patients and good for us.”