Vaccinations can stop delta variant
With delta driving more than 85% of COVID-19 cases in the U.S., vaccinations are the best path for ending the pandemic, says Carolina virologist David R. Martinez.
The United States should focus its vaccination and treatment efforts on the highly contagious delta variant of COVID-19 as it is driving the majority of cases in the U.S., Carolina vaccine researcher David R. Martinez says.
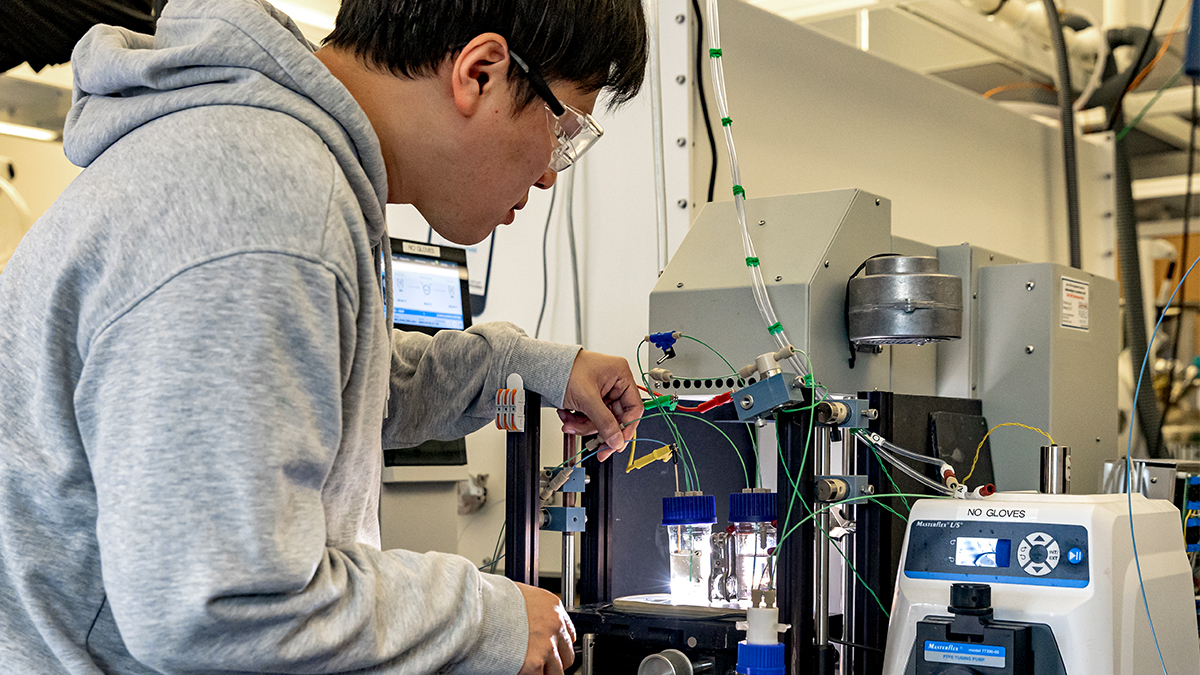
Martinez is a virologist on a scientific team at Carolina developing a universal vaccine that could be effective against the COVID-19 SARS-CoV-2 virus, its variants and related zoonotic coronaviruses. Zoonotic viruses are those that jump from non-human animals to humans. The vaccine uses messenger RNA similarly to the Pfizer and Moderna vaccines, but instead of using mRNA code to target only one virus, it combines mRNA from multiple coronaviruses to combat multiple variants and zoonotic viruses. Research shows that the vaccine protected mice from SARS-CoV-2 coronavirus, the beta variant, the early 2000s SARS coronavirus and coronaviruses that have not yet jumped from animals to humans.
A Hanna H. Gray Fellow at the Howard Hughes Medical Institute, Martinez is a postdoctoral researcher in the laboratory of Ralph Baric, an epidemiologist at UNC Gillings School of Global Public Health and professor of immunology and microbiology at the UNC School of Medicine. Baric’s research has led to new therapies to fight infectious diseases.
In a conversation with The Well, Martinez discusses delta’s ability to spread, how vaccines replicate our body’s natural defenses, what effect a universal vaccine might have on the pandemic and more you need to know about COVID-19.

David R. Martinez
What should people know about delta?
The main thing about the delta variant that we’re seeing is its increased transmissibility relative to previous variants. A person with the original strain might likely infect one or two people in a close setting, but someone with delta could infect four to six people.
How do scientists know that people infected with delta shed the virus at higher rates?
The science behind that knowledge is observational studies in several different locations in the country. The Centers for Disease Control and Prevention has looked in detail at a number of clusters of outbreaks. For example, some of the primary data that the CDC examined were based on a community outbreak among vaccinated people in Massachusetts.
They determined this by physically sampling for viral nucleic acid in the airways of fully vaccinated and unvaccinated individuals and found that they had similar levels of viral RNA in the upper airways. They measured this by a PCR [polymerase chain reaction] test where you swab each nostril, then the sample is sequenced. The sequencing determines if there’s virus nucleic acid and, if so, what lineage does this specific virus correspond to? Is it delta, is it epsilon, etc.?
How should anyone infected with delta or any other variant react?
I will caution that the presence of viral nucleic acid in the nose does not necessarily mean severe disease. The COVID-19 vaccine has the same goal of most, if not all, vaccines: to prevent severe disease from any virus. Of course, the aspirational goal or standard is to prevent disease altogether, but with a lot of vaccines, you don’t necessarily need to be protected from infection, but you just need to be protected from a severe form of the disease.
The virus has mutated. Now it’s more transmissible. There are even breakthrough cases in vaccinated people, but if the vaccine prevents ICUs from being overwhelmed, then the vaccines are working.
What else do people need to know now about variants?
Lambda appears to be dominating infection in South America. It has been for the last few months. And who knows what it will do? That is hard to predict in an ever-changing pandemic. What we saw with alpha at the first of 2021 is that it dominated infections in several parts of the world, but it now seems to be overtaken by delta.
The vast majority of cases in the U.S. — greater than 85% — are delta. This does not mean that the other variants are not important, but in our part of the world, non-delta variants are currently not as concerning.
It’s important that people know that none of what we call “scariants” or variants that scare people, have, so far, completely evaded vaccine-elicited antibody or immune responses. That’s true for them all — alpha, beta, delta, epsilon, lambda and so forth.
We see a dampening in the level of immunity as far as immune recognition and something that we call neutralization, which is a biomarker that for mRNA vaccines can predict whether someone develops clinical disease or not. The mRNA vaccines raise that biomarker to high levels.
If you’re healthy and do not have a comorbidity or risk factor associated with severe COVID-19, you’re still protected in most cases. The COVID-19 vaccines, in most cases, provide immunity at a much higher level than the body’s reaction to a natural infection. Some people who get a natural infection make high antibody levels, but the vaccine seems do that more consistently in most people.
As variants emerge, what’s our best path to ending the pandemic?
Vaccinations. When I evangelize for the vaccine, I always talk about diseases like measles and polio. You don’t hear about those diseases anymore because of highly effective vaccines. Poliomyelitis has practically been eliminated from the United States and other parts of world because of vaccinations, barring exceedingly rare, imported cases from travel. Polio has been eliminated in most of the world, with the exception of a few countries in the Middle East that have rare and sporadic outbreaks.
Similarly, some people may not know about rubella, and that’s because the MMR vaccine — measles, mumps and rubella — has reduced cases so dramatically. It’s one of the standard pediatric vaccines as well as for women of childbearing age. The “R” in MMR stands for rubella. You don’t hear about congenital rubella infection anymore, as was once more common before the vaccine, because the MMR is highly effective.
So, does that mean we can expect a time when the pandemic ends, or will it become more like seasonal flu outbreaks?
It will end someday. What will it take? Not just a lot higher vaccine acceptance, but I would say once we reach a high enough number of people who are naturally infected and vaccinated, then we’ll have a wall of immunity that’s going to prevent rampant spread of the virus. As far as knowing if it will become similar to flu outbreaks, that is anybody’s guess.
With COVID, we are certainly learning as we go, and we are making the most informed and educated decisions based on the data we have. The data have to drive our decisions if we want to have a chance to control and contain the pandemic.
What else is important for people to know about how vaccines work and your search for a universal vaccine?
Developing mRNA vaccines is one way the human brain really shines by taking a natural system and reapplying it.
Every cell in your body makes mRNA at all times to carry out basic biological functions. That is literally how your cells survive and carry out their functions. Your cells in the brain, cells in your foot, cells in your heart. That is what they do.
It’s a biological system — in plants, amoebas, really in anything that’s alive. That is a required feature of life. So, mRNA vaccines are just borrowing a basic biological process that your body does already in order to survive.
I’m not sure a universal vaccine would necessarily eliminate COVID. I’m skeptical that the acceptance of a universal vaccine would be better than that of the Moderna, Pfizer or Johnson and Johnson vaccines.
A caveat with any universal vaccine concept is that we do not yet know how “durable” the responses would be or how long they would last. We do know that a universal vaccine like ours could have more broad protection against more genetically diverse coronaviruses. However, the current SARS-CoV-2 vaccines are excellent and could help control the pandemic if enough people were vaccinated.