Moments of clarity
In the past, cochlear implants were employed in people with severe hearing loss, improving their ability to hear the conversations around them. But now, studies show that these devices offer benefits to patients with mild or moderate hearing loss.
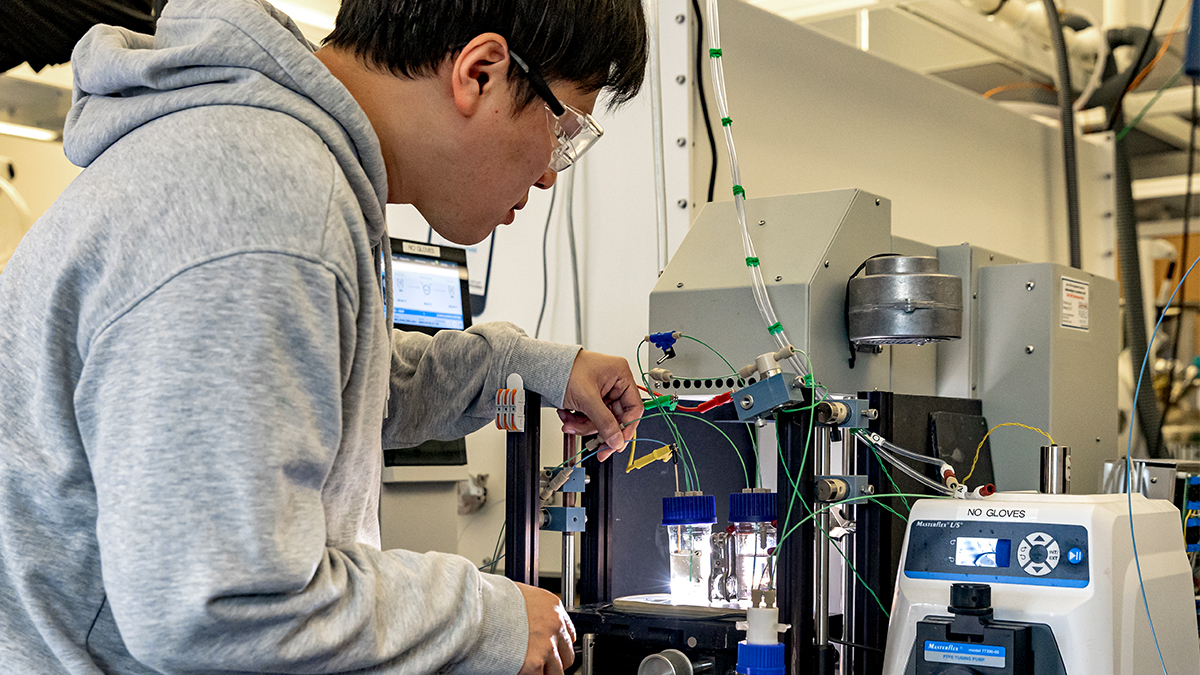
A semicircle of stereo speakers surrounded George Schneider*, who sat with his hands folded in his lap in the middle of a small, soundproof room.
A woman’s voice emitted from one of the speakers: “I just need a little air.” Schneider repeated the phrase. “Take a wild guess.” Schneider repeated that phrase too.
Gradually, more voices joined in from the various speakers, talking over the woman. “The engagement was not official.” Schneider, in his 60s, squints his eyes as he tries to concentrate. “Something artificial?” He was less sure. The room sounded like a crowded party layered with dozens of voices.
Schneider, who has a hearing aid in one ear and a cochlear implant in the other, is participating in a UNC-Chapel Hill clinical trial exploring indications for cochlear implants. Unlike hearing aids, which amplify sound, an implant helps restore speech perception. A patient needing one may be able to hear one-on-one conversations, but struggle to follow conversation among background noise.
“I don’t think that most people who have good hearing recognize what impact not having it has,” said Kevin Brown, medical director of the Children’s Cochlear Implant Center at Carolina. “It becomes very isolating and really affects quality of life.”
Previously, cochlear implants were predominately used for people with poor hearing in both ears, as outlined by the Food and Drug Administration and many insurance companies. If a patient had a lesser degree of hearing loss or single-sided deafness, there weren’t many options.
“Patients were told if they had one normal hearing ear that was good enough,” said Margaret Dillon, director of the UNC-Chapel Hill cochlear implant clinical research program. “Now we know that hearing in one ear is not good enough. There are options that can restore that hearing.”
Evidence points out a correlation between hearing loss and increased social isolation, depression and fatigue, Brown notes. Most recently, it has also been associated with accelerated cognitive decline, like dementia. Among children, hearing issues can lead to difficulty in learning and behavior problems.
Researchers at the UNC Adult Cochlear Implant Program and the Children’s Cochlear Implant Center explore these expanded indications. Around 70 patients have participated in a total of six clinical trials thus far, completing a variety of auditory tests every few months for one year after implant activation. Among participants, researchers have seen significant improvements in speech perception, ability to localize sound and better quality of life reports.
“Over the course of time we appealed to the FDA and said, ‘You know, these things are good for people you don’t even know they’re good for,’” said Harold Pillsbury, emeritus chair of the UNC School of Medicine’s Department of Otolaryngology/Head and Neck Surgery. “We need to include these people in the network of candidates so that they can get help.”
Opening up the world again
Cam and David Halstead lean over their living room coffee table, sifting through boxes of old photos. David picks up a family portrait. Seated in front of a fireplace, each member is wearing matching royal blue sweaters — a popular motif of the ’90s. In another, two young girls stand in front of a large bush covered in flowers. The two are either squinting at the sun or cringing at the fact that they’ve been instructed to put their arms around one another — it’s hard to tell.
“Oh, these are great shots,” David said. “See, that’s the first house.”
Cam picks up a portrait of a baby in a blue striped jumper, a bow around her neck and teddy bear in her lap. “This is Allie at 6 months,” she said, pointing to the photo.
Almost a year after the birth of the Halstead’s fourth child, Cam contracted a virus that resulted in hearing loss. She was fitted with two hearing aids, but they didn’t help. Because she was still having issues with word recognition, Cam stopped wearing the hearing aids and did her best to avoid situations that would obstruct her hearing.
In 2005, David was diagnosed with Meniere’s disease, causing hearing loss, tinnitus, and intense vertigo. This made avoiding hard-to-hear environments difficult for both, especially since David’s job involved social events, and Cam was expected to join in.
“If we were at a table of like 10 people having dinner, we would have to sit with our bad ears next to each other, therefore focusing all the attention on our good side. It was convenient because it was my right ear and her left ear,” David joked. “If it would have been two left ears it would have been like having two left shoes.”
Other aspects of their life were affected too. With four children — now adults and with children of their own — family gatherings were challenging. They also struggled to do the activities they loved as a couple: traveling, going to restaurants, and attending operas, concerts and movies. Even day-to-day conversation between them was hard.
“I was repeating myself at least twice, if not three times,” David said. “It was very frustrating, and that’s coming from someone that should be pretty sensitive to it because I was going through this myself.”
After several attempts to alleviate symptoms from Meniere’s disease, David had a labyrinthectomy and cochlear implant surgery in 2017 as a patient in the clinical trial.
“What I hadn’t really counted on was being able to hear again,” he said. “I had not really heard well out of my left ear in 17 years and, you know, it sort of opened up the world again for me. And that was delightful.”
Seeing David’s successful surgery convinced Cam to have her hearing tested again. Doctors found she had hearing loss in both ears and qualified to be a participant in the clinical trial. She underwent cochlear implant surgery in 2019.
Implantation is just the first step of a long road to hearing. When patients have their devices activated, many report that sound comes through as beeps or is distorted in pitch.
“It was very strange. The audiologist’s voice, when it came through it sounded like the ‘Looney Tunes’ Martian,” Cam explained. “Every syllable was a beep, so I had to focus on whatever the word was underneath the beep.”
Over time, Cam’s brain will adjust to the implants and correctly interpret incoming sound. Until then, it’s all about practice.
“It’s such great technology. It’s great for 65-, 70-year-olds. It makes a huge improvement in your quality of life,” David said. “But, you know, putting them on children at that first-year point or as early as they can when they’re born deaf is really kind of a miracle.”
Starting off strong
Alex and Fruzsina Deli stand in the waiting room of the Children’s Cochlear Implant Center at UNC-Chapel Hill, their 8-month-old son, Mason, sitting contently between the first-time parents. Two months earlier, Mason underwent cochlear implant surgery. Today, his device will be activated.
The door to the exam area opens, and a teenager and his parents walk into the waiting area. The boy chats with the receptionist and jokes with his father while his mother schedules another appointment. Alex and Fruzsina exchange a hopeful glance, noting the ease with which the young man is able to communicate. Fruzsina’s brother experienced hearing loss when he was young, and still has difficulties conversing with others.
“He has a hard time speaking,” Fruzsina said. “I was afraid Mason wasn’t gonna be able to speak as we, or he’s not gonna understand people, or people are not gonna understand him.”
The Delis knew Mason had difficulty hearing early on, after failing multiple newborn hearing tests. They were told that a hearing aid may help somewhat, but a cochlear implant would be more effective.
“We had two options,” Fruzsina said. “He is gonna be deaf the rest of his life or we are gonna do the surgery. And it was easy [to decide] because I want him to hear. I want him to hear everything. It was easy, but it’s scary, too.”
Alex’s insurance required Mason be at least 1 year old to undergo surgery, but the couple feared waiting that long would hinder his development. Luckily, Mason qualified to participate in the UNC clinical trial and underwent surgery when he was 7 months old.
On activation day, Mason sits in a highchair in the exam room. An audiologist explains the ins and outs of the devices to the Delis — from how to power them on and off to cleaning and tricks to keep them attached to their toddler’s head. Finally, it’s time. The audiologist turns on Mason’s implants, starting off at the lowest volume and incrementally working her way up.
Happily playing with a toy, Mason doesn’t initially notice anything. His attention eventually shifts, though, and he becomes still. Confusion creeps across his face as he begins to register the sounds. He breaks out in a cry. Concerned, Alex and Fruzsina look to the audiologist, who reassures them this is a normal reaction among young children — he’s experiencing sound in a way he never has before.
A few months later, Mason is back in a highchair but, this time, in his family’s living room. Fruzsina sits behind her son, holding a toy airplane. She reaches around, dipping and turning the airplane in front of Mason. “Ahhhhhh,” she said. Mason’s eyes follow the plane and he grabs at the toy. “Ahhhhhh,” he repeated, and Fruzsina laughed.
The two are practicing Mason’s speech development. Every week, a UNC-Chapel Hill speech language pathologist visits to check his progress, practice speech and hearing, and teach new exercises.
In the four months since Mason’s activation, his parents have noticed subtle yet promising changes in his hearing abilities. He turns his head to better locate curious sounds, responds to his name, and bangs on surfaces to see what noise will ensue. Once worried about their son’s future, the Deli’s now anticipate him communicating with ease — just like the teenager they saw months ago at the doctor’s office.
*Patient’s name has been changed for privacy.