Beating cancer shouldn’t mean the end of care
Mentoring the next generation of health providers is key, she said. “Being at a university like UNC is a wonderful opportunity to do that at the same time we are delivering cancer care to patients and conducting research to improve that care,” she said.

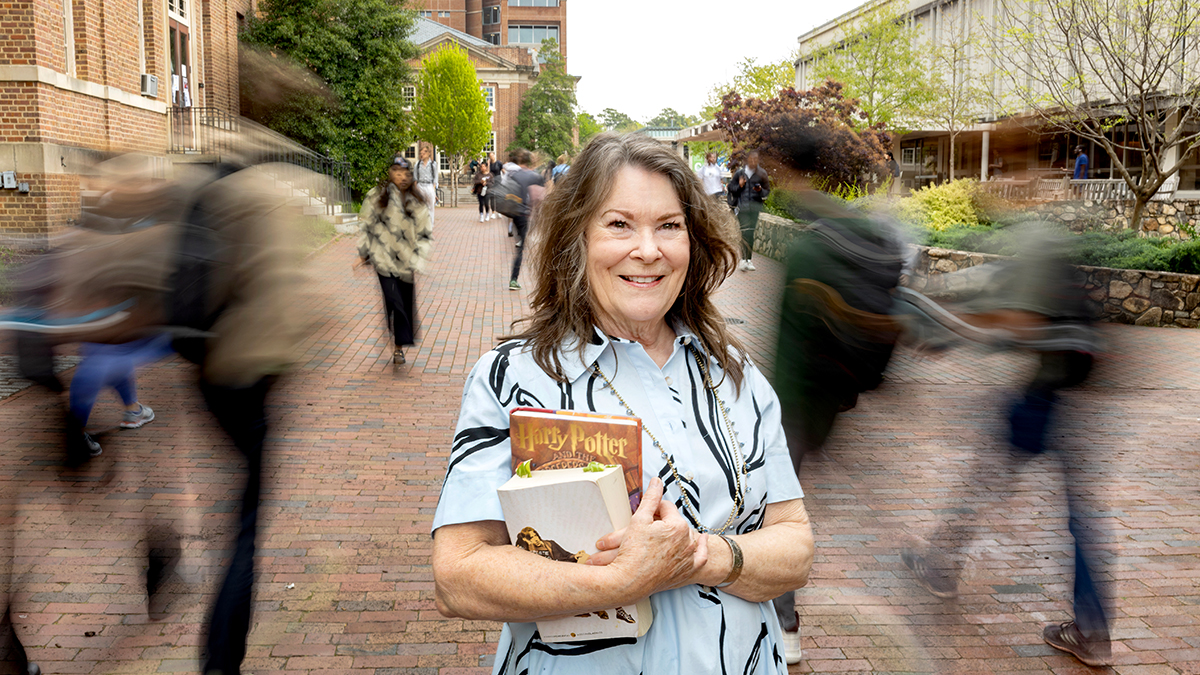
A registered nurse and professor in the School of Nursing, Deborah Mayer is also a national pioneer in research on cancer survivorship. Earlier this year, she was named director of cancer survivorship at the UNC Lineberger Comprehensive Cancer Center, where she leads the effort to enhance clinical and research initiatives for cancer survivors.
Mayer is a breast cancer survivor herself, for seven years now, but she’s quick to point out that her research interest grew out of her 40 years as an oncology nurse. For the relatively few patients who survived cancer that long ago, “we had a sort of ‘treat ‘em and street ‘em philosophy,” Mayer said.
But newer and better methods for early detection and treatment mean that an estimated 14.5 million Americans are cancer survivors – and can’t be simply dismissed without further monitoring and management.
“Now we know there needs to be surveillance for the cancer coming back and surveillance for side effects and late effects of treatment,” Mayer said. “Anything strong enough to treat a cancer is going to have some residual effects for many people. At least a third (of cancer patients) can experience significant long-term late effects.”
A 2006 Institute of Medicine report, “Lost in Transition,” recommended the creation of survivorship care plans. Recognizing the need for such plans was a major step forward for survivors, Mayer said, but medical professionals found it too complicated and time-consuming to put the plans together. They also couldn’t bill for that time, so very few care plans were being written and delivered.
To address the problem, Mayer chaired an American Society of Clinical Oncology work group to design a care plan with the patient in mind. The four committee members thought like patients and pared down the complicated plan to focus on what patients and their primary care providers wanted and needed to know. During the two-year process, the committee cut 80 percent of the original content and then pilot-tested the new version.
The result is a streamlined form – one page, front and back – that not only sums up the patient’s past problems and treatments, but also tells the patient what to expect next, what is considered normal and what should trigger a visit to the doctor.
Ramping up communication
Mayer is also pushing for better communication among oncology medical staff, patients and their primary care providers, starting with the diagnosis, especially since patients and their families often don’t hear anything the doctor says after the word “cancer.”
“Even if you’re a health-care professional, you become a bucket of Jell-O when it’s your turn,” she told a roomful of participants in “Cancer and Older Adults,” a public forum held recently at the Friday Center. “And it’s going to be our turn eventually.”
A cancer diagnosis is overwhelming and frightening, she said, and patients generally absorb only about 10 percent of what the doctor tells them at the time. But they shouldn’t feel rushed to make decisions.
“In many cancers there’s time to take a deep breath, there’s time to figure out what’s going on, there’s time to get a second opinion,” Mayer said. “There’s time to learn more before making your decision, because your first treatment is your best treatment, and you don’t want to have regrets later on.”
She urges patients to be active in their care, to write down their questions before going to see the doctor and to record the answers or have the medical professional write them down. Medical professionals also need to drop what Mayer calls “onco-speak.”
“If you can’t explain things in a way that your grandparents could understand, “ she said, “then you’re probably making it too complex.” At each visit, the oncologist should “ask, tell, ask.” Ask if the patient has questions, tell the patient what’s happening next and why, and then ask the patient to repeat what’s been said to ensure the information is understood.
The patient’s perspective
Mayer also wants medical professionals to see the situation from the patient’s perspective. Having been an oncology patient herself, Mayer said she’s more sensitive to her patients’ concerns. She provides plans outlining when and how they will get test results. She considers what it will mean to them if she orders one more test: Will they have to get off work? Do they have to drive a long distance? Will they need to find care for their children?
Great strides have been made in accommodating the needs of pediatric oncology patients, including how to keep them caught up at school during treatment, Mayer said, “but we have very little help or advice to people about how to keep their jobs.” Only recently has chemotherapy been offered on Saturdays or in the evenings to accommodate working adults, she said.
Even more difficult is learning to listen for the question behind the patient’s question.
Mayer tells the story of a patient who kept asking his doctors how much time he had to live. Not wanting to discourage him, they would say things like, “You’re doing fine,” or “Don’t worry.” But as the man persisted, Mayer began to drill down deeper into his question until she found out what he really wanted to know.
The man didn’t want a specific date. But he did want to know if he would have time to sell his house and move his family to a better part of town. He wanted to know how his illness would affect his young children and whether he would be able to stay at home at the end, or if that would be too scary for them.
“Anxiety and uncertainty go hand in hand,” she said. Once the man knew what to expect, he was able to make decisions for the end of his life that would be best for his family.
This kind of interaction is something Mayer treasures, which is one reason she spends a half-day each week seeing patients in addition to her research and teaching duties.
Mentoring the next generation of health providers is key, she said. “Being at a university like UNC is a wonderful opportunity to do that at the same time we are delivering cancer care to patients and conducting research to improve that care,” she said.
Mayer has seen many changes in cancer care during her career, including the development of better drugs to prevent nausea and relieve pain, although there is much more work to be done.
She thinks the future will bring greater involvement of primary caregivers in the care of survivors, more collaborating teams of oncology professionals, and primary care providers and patients who are more willing to ask the really hard questions.
With baby boomers like herself aging out of the workforce, Mayer hopes that more health professionals will specialize in oncology.
She points to a memory book displayed in her Carrington Hall office, printed for her by her latest class of nurse practitioners in oncology, and smiles. “I want to train the next generation so I can retire.”
To read more about Mayer’s work, see go.unc.edu/r4N8B.