Bioelectronics meets medicine
Assistant professor Wubin Bai and his team have developed a novel, bioelectronic technology that will improve patients’ lives, helping to safely automate and lower the burden of post-recovery care.

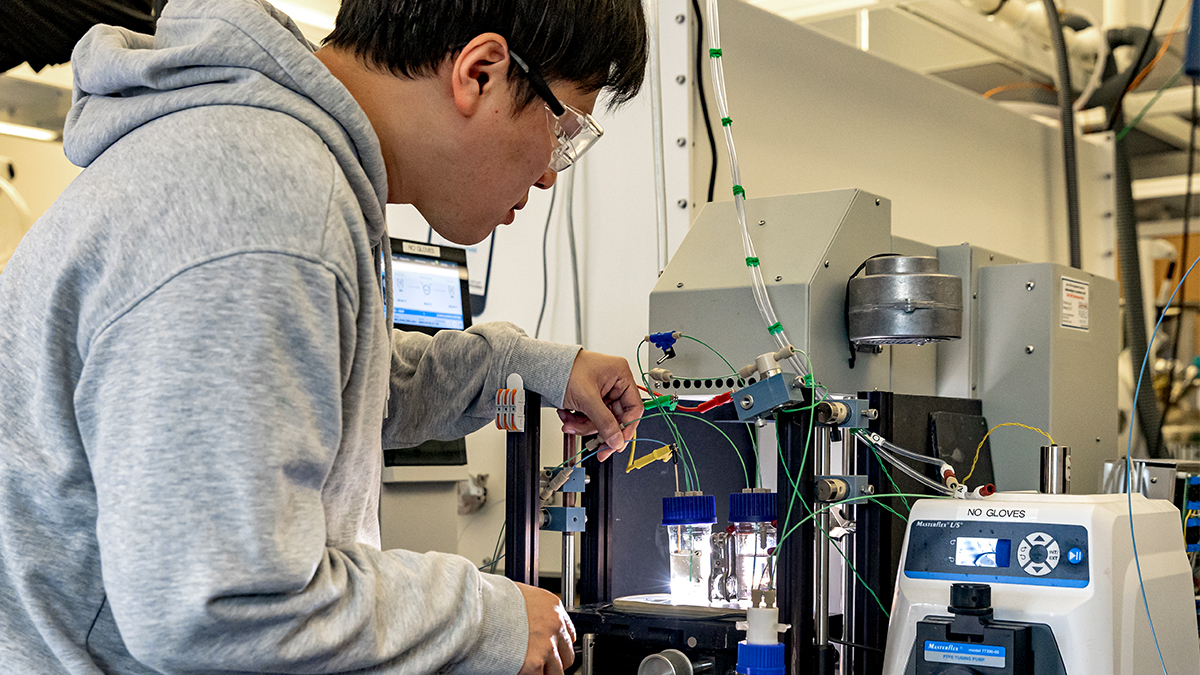
When Wubin Bai formed his lab, he was determined to incorporate and cultivate a culture of collaboration. An assistant professor in the department of Applied Physical Sciences at the University of North Carolina at Chapel Hill, Bai infuses this approach throughout his work. His team of multi-disciplinary graduate and undergraduate students – from APS and the UNC School of Medicine – is gaining attention for their novel wireless sensing patch that reduces tissue damage post-surgery, while improving user comfort compared with implantable deep-tissue monitors.
“Working with researchers from different backgrounds adds more possibilities along the research journey,” says Bai. “Having different backgrounds can provide a source of ideas from different perspectives, which can spark important moments.”
The sensing patch is a wearable, wireless patch for deep tissue monitoring of biometric indicators, including heart pulsation and respiration, the amount of oxygen in the blood (pulse oximetry), and the amount of oxygen in body tissues (tissue oximetry). With its wireless capabilities, the sensing patch allows clinicians to monitor patients remotely and in real-time, which can lead to improved health outcomes.
And because it is wearable, the sensing patch reduces tissue damage and improves patient comfort compared with implantable monitors when it comes to the need for deep-tissue monitoring. In addition, the patch can simultaneously provide local and global physiological information.
“We think the sensing patch we developed can open up a new opportunity for muscular monitoring,” says Bai, who came to UNC Chapel-Hill in 2021. “Traditional wearable electronics can capture pulse oxygenation or track walking distance or exercise intensity. But we wanted to make a device that could capture the local tissue region, especially deep inside the skin instead of just the skin interface. The sensing patch can benefit patients who may have had a complicated procedure or may have a higher chance of infection and inflammation.”
So how does it work? For example, patients who suffer tragic incidents sometimes require muscle flap transfers. In these cases, the reconstructed flaps need close monitoring by clinicians to ensure the newly transferred tissue will become integrated into the neighboring tissues. Existing strategies for post-surgery care rely only on physical examination and external doppler tests – both of which are limiting as they depend on the skills of bedside personnel who must continuously check the transferred flap. However, the skin-interfaced patch developed by the Bai lab uses microneedle waveguides that overcome light scattering and absorption associated with skin and fatty tissue – allowing medical providers to assess health and healing deep within the tissue.
“The sensing patch and its wireless syncing capability allow for continuous monitoring and can immediately alert clinical personnel of any issues. This allows the recovery to become more automated, lowering the burden of post-surgery monitoring or post-surgery care,” says Bai. “The wireless sensing patch provides a safe, real-time, less invasive and low-cost way of recovery monitoring for flap-transfer surgery.”
Bai’s team recently had its paper “Skin Interfaced Deep-Tissue Sensing Patch via Microneedle Waveguides” about the technology published in Advanced Materials Technology.
“This is my first paper as a senior correspondent author and principal investigator, so that means a lot to me personally,” says Bai. “As professors, it’s motivating that we can form a team to make something publishable. It gives us confidence that we can put our passion into action and demonstrate our ideas to make an impact.”
Collaboration with the UNC School of Medicine provided Wubin and his team with the insight they needed to figure out if they could use current techniques in the lab to create the solution, or if they should explore additional techniques to solve the challenges they faced.
“Connecting with different areas of research outside APS tremendously benefited the team and the work,” says Bai. “Collaborating with the clinical doctors at the medical school was huge. The collaboration was very smooth and easy, and I was amazed by the passion of the team.”
As an undergrad, graduate and postdoc researcher, Bai had great experiences working in a collaborative environment with multidisciplinary teams. Today, he incorporates that same approach into his lab with his students.
“Sometimes, even a small and unintentional suggestion from a researcher of a totally different field can save months of time in figuring out a way around a technical hurdle,” Bai says. “Collaborating with UNC medical experts, especially doctors on the front line, helped us learn more about their personal experiences with the existing medical instruments as well as the potential challenges we might face.”
Bai is working with Innovate Carolina’s Office of Technology Commercialization to move the technology forward, and the team has a provisional patent filed associated with the paper. OTC helps accelerate the translation of important ideas into meaningful products and services for the benefit of North Carolina, the world and the University. Bai hopes the technology can be available in the near future to address overall unmet medical needs and challenges.